Why 18G is thicker than 22G explained


When people first encounter medical needles, one common question arises: why is an 18G needle thicker than a 22G needle? At first glance, this seems backwards. Shouldn’t a larger number mean a larger diameter?
Most clinicians, nurses, or patients accept this as a given rule without thinking too much about it. But the truth is, this “counterintuitive” numbering system actually has its roots in 19th-century British wire manufacturing.
Back then, wire makers used a process called wire drawing—pulling metal rods through progressively smaller holes to reduce their diameter. Each time the wire was drawn thinner, the process step was recorded as a new “gauge.” The gauge number was not the measurement of the wire itself, but simply the count of drawing stages.
This means the more times a wire was drawn, the higher its gauge number became, and the thinner the final wire. When the medical industry began producing fine stainless steel tubing for hypodermic needles, it directly adopted this gauge numbering method. That’s why, to this day, the larger the gauge number, the thinner the medical needle.

The “G” in needles stands for gauge, usually referring to the Birmingham Wire Gauge (BWG) system.
Definition: Gauge in medicine refers to the outer diameter (OD) of a needle tube.
Direction: A higher gauge number corresponds to a smaller outer diameter.
Uneven increments: Gauge steps are not evenly distributed. They are the legacy of workshop practices, not a precise mathematical sequence.
For example:
An 18G hypodermic needle has an OD of about 1.20 mm. A 22G needle has an OD of about 0.70 mm. So even though 22 is numerically larger, the 18G needle is physically thicker.
Since early hypodermic needles were developed directly from fine metal wire and tubing, manufacturers naturally used the gauge system already familiar in industry. The medical field inherited this language and continued using it.
Gauge became a global common standard for suppliers, manufacturers, and clinicians. If a surgeon in the U.S. orders a 20G Puncture Needle, the supplier in Asia instantly knows the exact OD required. This eliminates miscommunication in international procurement.
Today, gauge has been fully incorporated into international standards:
ISO 9626 defines stainless steel tubing for medical needles (10G–34G).
ISO 6009 assigns a color-coded system for disposable injection needles, ensuring quick visual recognition and reducing medical errors.
Thus, what started as a workshop shorthand is now a fully integrated, standardized part of global healthcare.
To understand this paradox, imagine a 19th-century Birmingham wire workshop.
Metal rods were drawn through a sequence of progressively smaller dies. Each pass reduced the diameter and was marked as one step in the gauge system. Importantly, the number didn’t reflect the actual diameter—it simply indicated how many drawing steps had been completed.
When medical needles emerged, the industry adopted the same numbering sequence. Over time, those historical stages became embedded in medical standards.

In medical applications:
Gauge = outer diameter (OD).
Inner diameter (ID) depends on wall thickness.
For instance:
A 22G standard-wall needle has a smaller ID than a 22G thin-wall needle, even though both share the same OD.
This directly affects fluid flow rate, aspiration efficiency, and injection comfort.
18G ≈ 1.20 mm OD
20G ≈ 0.90 mm OD
22G ≈ 0.70 mm OD
French (Fr) is used mainly for catheters: Fr = OD (mm) × 3.
Gauge, however, is non-linear and cannot be directly converted.
As a rule of thumb:
18G ≈ 1.20 mm OD
4 Fr catheter = 1.33 mm OD
Two international standards keep the system reliable:
ISO 9626: Defines stainless steel tubing sizes, mechanical strength, and wall thickness categories for needles (10G–34G).
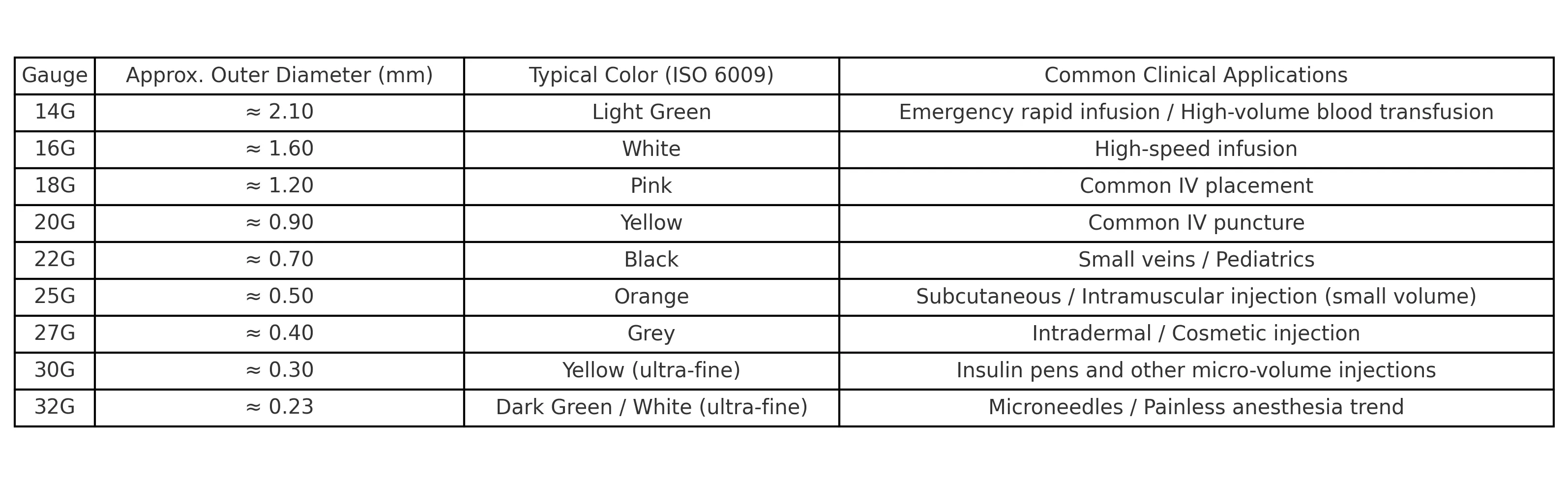
ISO 6009: Defines a universal color code (e.g., pink for 18G, yellow for 20G, black for 22G), helping clinicians select the right needle instantly.
Together, they act as safety locks, ensuring that gauge remains consistent and safe worldwide.

Always specify OD, gauge, and wall type (e.g., “22G × 0.72 mm, thin wall”). Avoid writing only “22G.”
Adhere to ISO standards when documenting, purchasing, or designing. Include tolerances and color codes.
For high-flow needs, consider thin-wall or extra-thin-wall needles. Remember, wider ID increases flow but may reduce mechanical strength.
Gauge is not just an engineering number—it influences patient outcomes. Different procedures require different needle gauges:
Hypodermic Needles – For injections, thicker gauges (e.g., 18G) are used for rapid infusion, while finer gauges (e.g., 25G) are chosen for comfort and precision.
Puncture Needle – Gauge size affects penetration force and sample retrieval efficiency in diagnostic punctures.
Chiba Needles – Often used in biopsies and fine-needle aspirations, where thinner gauges allow precision while minimizing tissue damage.
Endoscopic Biopsy Needles – Gauge balances tissue sample size with patient safety during endoscopic ultrasound-guided biopsies.
Spinal Needles – Gauge selection impacts cerebrospinal fluid flow and patient comfort during anesthesia procedures.
These examples show that choosing the right gauge is both a clinical and engineering decision, balancing fluid dynamics, patient safety, and procedure efficiency.
The question of why an 18G needle is thicker than a 22G needle leads us back to 19th-century Birmingham wire drawing workshops. The system wasn’t designed to be intuitive, but medicine inherited it and later embedded it into international standards.
Today, gauge remains a global language in medical needle manufacturing. By understanding that gauge defines OD, while wall thickness affects ID, both clinicians and engineers can make precise and safe choices.
From injections to biopsies, punctures, and spinal anesthesia, gauge size continues to play a critical role in medical practice.